Influence of Patient Transfer Network of US Inpatient Facilities on the Incidence of Nosocomial Infections
Abstract
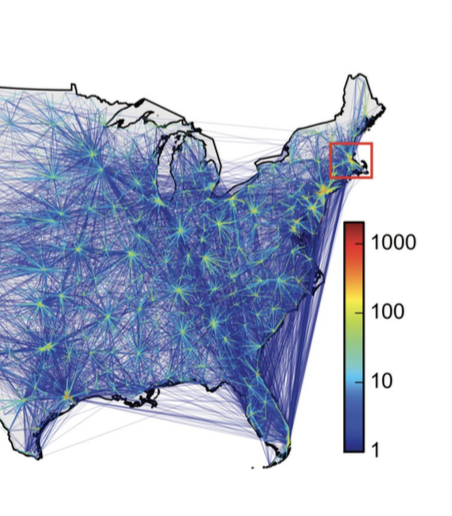
Antibiotic-resistant bacterial infections are a substantial source of morbidity and mortality and have a common reservoir in inpatient settings. Transferring patients between facilities could be a mechanism for the spread of these infections. We wanted to assess whether a network of hospitals, linked by inpatient transfers, contributes to the spread of nosocomial infections and investigate how network structure may be leveraged to design efficient surveillance systems. We construct a network defined by the transfer of Medicare patients across US inpatient facilities using a 100% sample of inpatient discharge claims from 2006–2007. We show the association between network structure and C. difficile incidence, with a 1% increase in a facility’s C. difficileincidence being associated with a 0.53% increase in C. difficileincidence of neighboring facilities. Finally, we used network science methods to determine the facilities to monitor to maximize surveillance efficiency. An optimal surveillance strategy for selecting “sensor” hospitals, based on their network position, detects 80% of the C. difficile infections using only 2% of hospitals as sensors. Selecting a small fraction of facilities as “sensors” could be a cost-effective mechanism to monitor emerging nosocomial infections.
Citation:
J. Gracia, J. Onnela, M. Barnett, V.M. Eguíluz, and N. A. Christakis, “Influence of Patient Transfer Network of US Inpatient Facilities on the Incidence of Nosocomial Infections,” Scientific Reports, 7: 2930 (Jun 2017) DOI: 10.1038/s41598-017-02245-7