Attitude and Self-Reported Practice Regarding Hospice Referral in a National Sample of Internists
Abstract
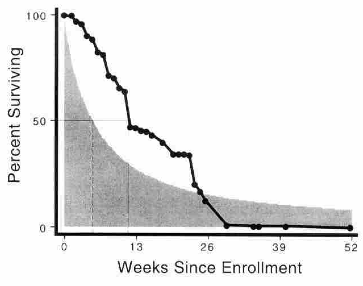
Systematic, nationally representative information about physicians' attitudes and behavior with respect to hospice care is not available. We sought to describe these previously unexamined attitudes and practices. We conducted a mail survey of a random national sample of 1311 internists, of whom 697 responded (an unadjusted response rate of 53%). We elicited physician's attitudes and self-reported practice with respect to hospice. Most internists (89%) felt that hospice care was a good form of terminal care. Physicians with longer definitions of what constitutes "terminal" illness and those whose patients were more accepting of their prognoses were more likely to hold this opinion. Over the course of a year, the median internist referred five patients to hospice. Specialists and those with longer definitions of "terminal" were more likely to have done so. When asked "if you knew exactly how long a patient had to live, how long before death would you refer them to hospice?" the average response was 12.1 +/-8.5 weeks, but responses varied from 1 to 52 weeks, and the pattern of responses was bimodal, with one peak at about 13 weeks (73% of internists) and one at about 25 weeks (27%). Moreover, the distribution of hospice enrollment times implied by physician reports about ideal practice is significantly more compact than the distribution of survival that is actually observed; physicians support far fewer very short (<2 weeks) and very long (>6 moths) stays in hospice than are observed. We conclude that internists show significant support for, and utilization of, hospice and they endorse a length of stay that is longer than currently observed. These findings suggest that it may be possible to increase both the number of patients using hospice and their duration of use of hospice.
Citation:
T.J. Iwashyna and N.A. Christakis, "Attitude and Self-Reported Practice Regarding Hospice Referral in a National Sample of Internists" Journal of Palliative Medicine, 1(3): 241-248 (September 1998)